2016
“Continuous exposure of pancreatic cancer cells to dietary bioactive agents does not induce drug resistance unlike chemotherapy”
Continuous exposure of pancreatic cancer cells to dietary bioactive
agents does not induce drug resistance unlike chemotherapy
P Fan, et al., Molecular OncoSurgery, University of Heidelberg,
Cell Death and Disease, 2016

Welcome!
“It becomes evident that excessive activation or insufficient control of complement activation on host cells can cause an immune imbalance that may fuel a vicious cycle between complement, inflammatory cells, and tissue damage that exacerbates clinical complications.”
Complement in Immune and Inflammatory Disorders:
Pathophysiological Mechanisms
Daniel Ricklin and John D. Lambris,
Journal of Immunology, 2013
Redefining chronic diseases and cancers
Regardless of the inconvenience, established medicine must recognize that the biology and cellular mechanisms of chronic disease and cancers have now been identified and validated with thousands of peer-reviewed, published research studies. Chronic diseases are distinguished by cyclic, escalating self-injury with concomitant tissue modification. Cancers, extreme versions of chronic disease, are not “invaders.” From the body’s perspective, its behavior at the cell level, cancers are actually wounds, wounds that are constantly being “re-injured.” When observed from this “new” perspective, our understanding of disease and opportunity to treat it changes dramatically. With this new understanding, brings new opportunity to investigate new approaches to healing (vs. killing).
What makes chronic disease “chronic”
Chronic diseases and cancers suffer from dysfunction in inflammatory response, which is the primary signaling mechanism of the body’s attempts to defend and heal itself. The inflammatory signaling cascade becomes amplified and cyclic, with each resulting in multiple feedback pathways, each pathway creating additional redundant signaling cascades, resulting in an exponential expansion of signaling. This very dynamic process not only restricts the body’s response to injury and healing, it also causes secondary injury. The body’s efforts to heal within this environment modifies tissues which can cause additional inflammation, additional symptoms and disability. It is also the reason why chemotherapy (including immunotherapy and cancer “vaccines”) treatments ultimately fail and create a more aggressive disease. The medical community has termed this phenomenon “treatment resistance.”
“Cell signaling pathways:” targets of therapy or sentinels of disease origins?
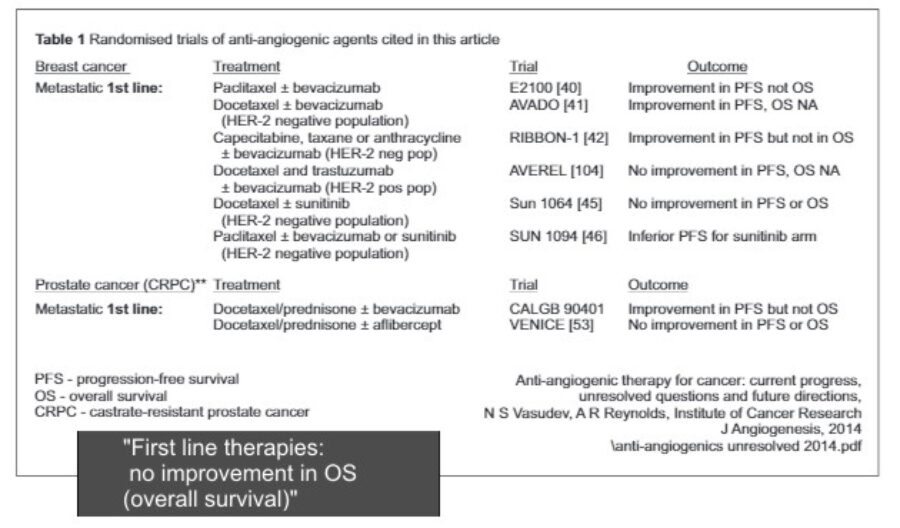
Cell signaling and signaling pathways are the sentinels of disease functions in the cellular microenvironment. This microenvironment represents the origin and engine of chronic disease. Should we treat the “messenger” or the cause? Chemotherapeutic drugs arguably treat only the messenger, to suppress or express a specific signaling agent or pathway. Isn’t it more reasonable to target the disease function at its origins? Apply agents that act in synergy with the body’s healing mechanisms? Chemotherapy continues to be a common strategy of killing or to obstruct healing. Will its legacy of failure continue into a future of low-expectations and fatalism? Regarding the following excerpt, this is what we can expect from the best that medicine has to offer? Each of the excerpts below are representative of the authors’ conclusions and are not taken out of context.
“But with cancer, where no simpler universal, or definitive cure is in sight – and is never likely to be – the past is constantly conversing with the future.”
“Future physicians may laugh at our mixing of primitive cocktails of poisons to kill the most elemental and magisterial disease known to our species.”
The Emperor of All Maladies, The Biography of Cancer, 2011
Siddhartha Mukherjee, MD, Oncologist
Pulitzer Prize, PBS documentary by Ken Burns
“Spontaneous, as well as (radiation) therapy-induced reprogramming of cancer cells is most likely subject to complex negative and positive feedback regulation and it remains to be investigated if the molecular mechanisms that underlie therapy-induced reprogramming are unique to cancer or if normal tissue damage repair employs the same pathways before it can be determined if this phenomenon has druggable targets with a therapeutic window.”
Cancer Stem Cells, Cancer Cell Plasticity and Radiation Therapy
Erina Vlashi and Frank Pajonk
Department of Radiation Oncology, David Geffen School of Medicine at UCLA
Comprehensive Cancer Center at UCLA
Seminars in Cancer Biology – Journal, 2015
Validation of nutritional agents
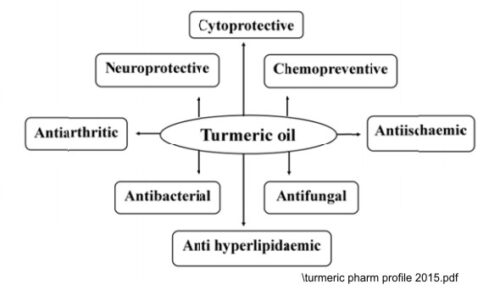
After thousands of years of knowledge without “scientific validation,” the cellular mechanisms of nutritional agents have been identified, pathways mapped, functions documented, results indisputable. In the example below describing the functional benefits of curcumin, if true (it is true), then why hasn’t medicine embraced this discovery, improved upon it and improved cancer and disease outcomes? If it is true and the medical establishment has chosen to ignore this capability, why hasn’t the general public bypassed medicine to pursue a scientific, disciplined approach to apply these agents and cure cancer and chronic diseases? Well, it is taking time, but that is exactly what is happening today. That is our objective to provide delivery protocols based upon science with specific, projected and consistent outcomes.
Nano-encapsulation technology
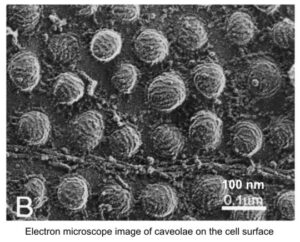
What if the particle of an agent to intended to treat a diseased cell was actually too large to be absorbed (endocytosed) by the cell? Electron microscopy has revealed that the cells in the disease microenvironment have very specific cell surface characteristics. Also, what if this nanoparticle was encapsulated in a material that naturally targeted the disease microenvironment? This technology has dramatically improved the “bioavailability” of nutritional agents.

“Silos,” the architecture of programmed disinterest
Over time, compartmentalization has occurred in medicine. The evolution of this medical culture has been consistent in medical research, in the development of pharmaceuticals and medical devices, and extends throughout the delivery of health care. Medical “specialties,” basic research and its associated financial grants encourage and support the culture of specialization. Diseases, their diagnoses and their treatments are defined according to each specialty. Participants are recognized and rewarded for their valuable work. However, due to nature of dividing medicine into specialties, the people involved at every level lack an a critical macro-perspective of disease, how the body as a system responds to injury, defends against disease and heals itself. Not only do they lack this critically important perspective (curiosity!), they lack the motivation to pursue conclusions or solutions outside of their specialty.
An ironic example of this system is the specialty of the macro-perspective of disease in society, called “epidemiology.” In the corporate world, this compartmentalization could be called “silos,” where production is focused (restrained) to a very specific category of product or service. In the established medicine culture, “family medicine” is the only medical specialty that pursues a global, whole body perspective. Even though a great community of physicians have committed themselves to a variety of versions of a whole-body approach to medicine, i.e. holistic, integrative, complementary, alternative, these sciences receive very little attention from academic institutions, hospital conglomerates or the leadership hierarchy.
So, for instance, if you ask, how many diseases do we now know the exact molecular basis? Turns out it’s about 4,000, which is pretty amazing, because most of those molecular discoveries have just happened in the last little while. It’s exciting to see that in terms of what we’ve learned, but how many of those 4,000 diseases now have treatments available? Only about 250. So we have this huge challenge, this huge gap.
Francis Collins, Director of the National Institutes of Health
TED Talks, 2012
Inherited “chronic” diseases
Would you be amazed to find that research has demonstrated that inherited genetic diseases are actually inherited “chronic diseases?” Recent published research has confirmed that epigenetic encoding of inherited chronic diseases can be reversed? Considering current efforts to “map the genome,” perhaps we should understand how the genome is extrinsically encoded, i.e. epigenetics.
Chronic diseases and cancers are curable
What happens when a disease is declared to be “incurable” or “terminal?” The sad reality is that physicians’ behavior toward you as a patient changes. The objective is no longer to cure your disease or cancer. The focus is to slow its inevitable progression or to ameliorate your symptoms. Drugs are FDA-approved even though they may only extend life a few months (and not for all patients!). It is expected that treatment therapies will eventually fail. It is now common to physicians to expect failure of a drug with another drug waiting in the wings to replace it. When physicians use terms like “hope,” or “if this drug fails, we can try another drug,” you must ask yourself, where is the science? How can medicine accept a very low standard? Except failure?
While prayer plays a critical role in healing, surviving and curing cancer is not about “hope.” The cure for chronic diseases including cancers has been identified, demonstrated and validated in a multitude of research studies. Cancer has been redefined. The cure for cancer, all cancers, all stages, is now in-hand. The agents and methods to defeat it have been identified. Markers, methodologies and devices have been developed to assess and monitor treatment. We must design the protocols to apply this knowledge.
Inherited chronic diseases
“Epigenetics describes the molecular factors that form complexes at regulatory regions of DNA to influence genetic activity without changing the primary DNA sequence. Such factors are usually inherited through mitosis but their meiotic (transgenerational) inheritance is controversial due to the expansive epigenetic remodeling that happens twice per generation – during gametogenesis and during very early embryonic development (64–66).”
The role of epigenetic change in autism spectrum disorders
Yuk Jing Loke, Anthony John Hannan and Jeffrey Mark Craig, Murdoch Childrens Research
Institute, Royal Children’s Hospital and Department of Paediatrics, University of Melbourne
Frontiers in Neurology Journal and NIH-NCBI, 2015
Epigenetic changes reversible
The reversibility of epigenetic aberrations has made them attractive targets for cancer treatment with modulators that demethylate DNA and inhibit histone deacetylases, leading to the reactivation of silenced genes.”
