Cell Signaling in Disease
“Studies on the two cellular stresses have opened new avenues to next-generation therapies for these debilitating illnesses.”
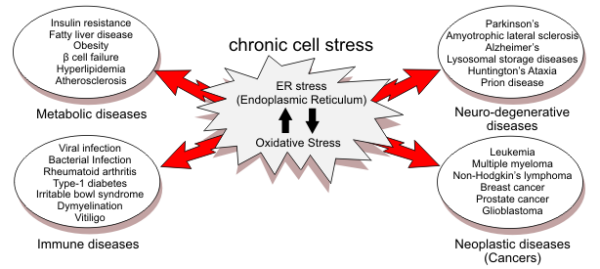
FIG. 5. ER stress and oxidative stress in human diseases. ER stress and oxidative stress are linked to multiple human pathologies, including metabolic, neurodegenerative, immune/inflammatory, and neoplastic diseases. Studies on the two cellular stresses have not only contributed to our understanding of the pathogenesis, but also opened new avenues to next-generation therapies for these debilitating illnesses. See ‘‘ER Stress and Oxidative Stress in Human Diseases’’ for details.
Adapted from: Endoplasmic Reticulum Stress and Oxidative
Stress in Cell Fate Decision and Human Disease
Stewart Siyan Cao, and Randal J. Kaufman, 2014
“The ability of metabolomics, particularly in combination with stable-isotope probing, to follow the metabolic fate of target compounds and their flux through specific pathways underlies its utility in the identification of new biochemical reactions occurring within cells. In this context, new pathways and metabolites can be identified without the need for targeted genetic modification or recombinant protein studies…”
Metabolomic strategies for the identification of
new enzyme functions and metabolic pathways
Gareth A Prosser, Gerald Larrouy-Maumus & Luiz Pedro S de Carvalho
Mycobacterial Research Division, MRC National Institute for Medical Research, London, UK, 2014
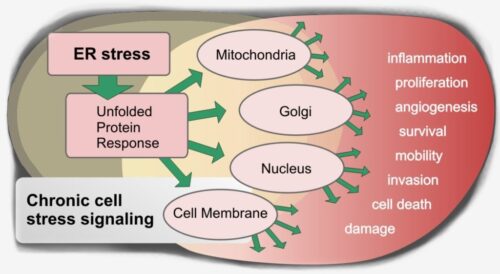
“Our current findings raise the possibility that UPR (ER stress-driven unfolded protein response) signaling can also regulate angiogenesis characteristic of atherosclerosis. It is possible that the ATF4 mechanism can supplement hypoxia-induced HIF-1 cascade, thus amplifying formation of neovessels in atheroma.”
ATF4-dependent transcription is a key mechanism in VEGF upregulation by oxidized phospholipids: O V Oskolkova, et al., Medical University of Vienna. 2008

Signaling Pathways
Cell signaling is the result of physiologic events in a functioning cell and its immediate environment. Signaling is represented by gene expression, DNA modifications, changes in metabolism, cell membrane, cell stress and damage, reactions to pathogens and other events, lipids, peptides, enzymes, proteases, and others.
Many researchers decry the complexity of physiologic signaling in the body which occurs as a response to disease. This signaling is generated at the cell level and in its immediate microenvironment. Each cell reacts to varying sources of stress or damage. Modifications occur in cell’s architecture, components, metabolism, the cell membrane and the extracellular space. The signaling is dynamic and continuous. It is a vast, redundant, interfering, reactive environment which is continuously, automatically responding to stimuli any one moment. Researchers have carefully mapped signaling pathways. The complexity of thousands of redundant and apparently conflicting signaling can only decoded if we examine the actual cell functions that generate the signaling. The cell functions generate signaling in response to a stress environment. These physiological events lead to signaling cascades which, in turn, elicit additional behaviors from other cells. It may well be a chaotic environment when considering gene expression and cell signaling, however, there is a great deal of evidence that cell function and signaling is very consistent among all chronic diseases and cancers. Cell signaling pathways have correlated with the genesis of chronic disease and cancer hallmarks, the classic identifiers of cancer.
There are two directions for medicine to proceed. To continue the current path, modifying or inhibiting cell signaling to obstruct cell functions, or to utilize cell signaling to understand and define cellular disease physiology. Investigation of specific cell functions under a stress environment, provides insight and understanding of disease at its very origins. The origins of cell signaling occur here. By addressing cell component functions, cell physiology, the opportunity arises to interrupt the injurious and perpetual cycle of inflammation and inflammatory response.
An abundance of recent research as clearly demonstrated that the signaling pathways of chronic diseases are dramatically similar. At the center of these pathways, are the agents of chronic inflammation and dysfunctional wound healing. There is also conclusive evidence that all chronic diseases and cancer share common characteristics. They also share the discovery of a physical substrate on the diseased cell’s surface that makes chronic diseases “chronic.”
We have been presented with the opportunity to cure previously incurable diseases. We now have the ability to clearly declare what is the definition of “cure.” No longer should we accept the low expectations of “cancer control” or insignificant, “increased survival.”
The only question is how established medicine will integrate this new-found knowledge into current practice. The track record has been mediocre at best. Chemotherapy drugs have received accelerated FDA approval to be administered to cancer patients. Results of these drugs have brought suffering and very high cost of care with little improvement in overall survival or disease-specific survival. Medical researchers readily declare that the cellular signaling environment is complex, redundant and adaptive. Yet, medicine continues to research, develop, approve and deliver drugs designed to inhibit or obstruct a specific signaling protein, only to be undermined by the disease through alternate signaling pathways. What was originally feared has been proven many times and continues today: these drugs inevitably create a more aggressive, more deadly cancer, resistant to the the chemotherapy drug originally administered.
