
Patient “LS,” a case study:
Diagnosis of localized prostate cancer, scheduled for surgery
LS, 58 years old, is scheduled with a Primary Care Provider, a Physician Assistant (PA), to establish with her as a new patient. He also needs to be given a pre-operative examination, approval of his provider that he is in good health for his scheduled prostate surgery. The PA began to review the patient’s history and reports from his urologist and biopsy analysis reports from the pathology lab. LS’s surgery to treat his prostate cancer was scheduled to occur in two weeks. The surgery was to consist of a complete resection (removal) of his prostate by a surgical procedure called a robotic radical prostatectomy.
Fortunately for LS, the PA’s office has initiated a program to improve screening and management for prostate cancer and prostate-related diseases like BPH (benigh prostatic hyperplasia) and prostatitis, an uncomfortable inflammatory condition in the prostate. While reviewing LS’s records, the PA became concerned that this patient may be scheduled for surgery prematurely. Even though this surgical procedure is common, there was not sufficient diagnosis in the record to justify such a dramatic solution as radical surgery and all of the side effects that come with it. As a primary care provider, the PA has responsibility for the patient’s entire health and well-being going forward throughout his life.
BPH and urinary symptoms
The reports revealed that the patient suffered from BPH with symptoms that included difficulty urinating and nocturia (waking at night to urinate). His prostate was unusually large, about 3 times the size of a normal prostate. His last serum PSA (prostate specific antigen) test revealed a level of 7.1 ng/ml. His highest PSA level was 10.1. This is higher than a typical patient for this age group, but actually a bit low for a man with such a large prostate. In addition, the patient had reported to his urologist that he was experiencing urinary symptoms and nocturia. At his age, elevated PSA and urinary symptoms, is not uncommon. It is pretty straight-forward to deduce that the patient had BPH, as elevated PSA and urinary symptoms are classic signs of the disease. The urologist’s reports confirmed that his prostate was enlarged. The PSA was more likely caused by BPH instead indicating risk of cancer.
Trans-rectal ultrasound-guided prostate biopsy
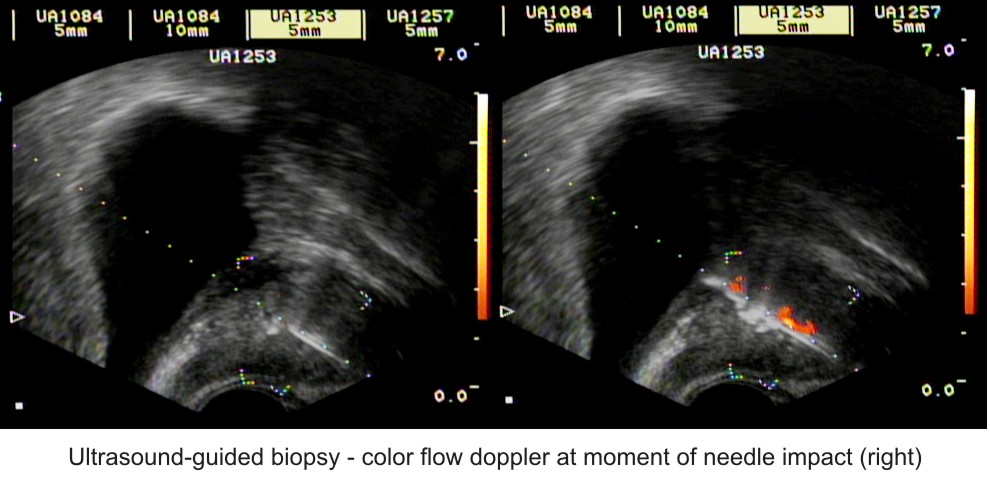
LS was diagnosed with prostate cancer after undergoing three prostate biopsy procedures. Once a patient is referred to a urologist, the method of diagnosis to determine whether a patient has prostate cancer is a procedure called a “trans-rectal, ultrasound-guided prostate biopsy.” And yes, as the name implies, it is exactly as is described. The urologist uses an ultrasound probe configured with a spring-loaded, needle biopsy gun and inserts it into the patient’s rectum. Due to the location of the prostate under the bladder and adjacent to the rectum, the probe can be positioned very close to the prostate. The procedure begins with the urologist manipulating the probe while imaging the prostate. The probe is positioned to various regions of the gland, the needle is released into the prostate and retracted with the harvested tissue. The urologist attempts to sample the entire prostate according to a template approach. The number of tissue cores typically “harvested” ranges between 8-12 cores. However, some urologists will take up to 18 samples or more. The procedure is very uncomfortable.
Review of the records revealed that LS had experienced this procedure on three separate occasions. Over a period of 4 years, LS had 3 biopsy procedures. The first biopsy failed to find any prostate cancer. The next year, there was no improvement of LS’s symptoms, PSA remained elevated. A second biopsy was performed. Results were again negative. In 2014, LS’s PSA had remained elevated and his symptoms persisted now for 4 years since first seeing his urologist. His urologist performed a 3rd biopsy procedure. This time, one of the tissue cores contained a tiny fragment of tissue, 0.8mm length x 1.0mm core diameter, that was identified as a low-risk, Gleason 6 cancer. Such a small volume of a single-core of low-risk cancer meant LS was an excellent candidate for surveillance. At minimum, he could delay surgery for several months or more for observation. According to research, there just wasn’t any real danger of any meaningful progression or risk to his survival. LS has now suffered 3 biopsies totaling 24 tissue cores harvested. On the third attempt, a single 0.8mm length of tissue core was discovered to contain low-risk prostate cancer.
“Although they may ultimately decide on treatment, there is no apparent gain to making this management decision quickly with the belief that a delay will compromise cure. Second, when selected carefully by use of criteria that suggest the presence of small-volume, lower-grade cancer and then monitored with a rigorous protocol for disease progression, these patients appear to have the same risk of non-curable prostate cancer for at least 2 years after diagnosis as those patients who received immediate prostate cancer surgery.”
Delayed Versus Immediate Surgical Intervention and Prostate Cancer Outcome
Christopher Warlick , Bruce J. Trock ,Patricia Landis , Jonathan I. Epstein ,H. Ballentine Carter
Brady Urological Institute, Johns Hopkins
Journal of the National Cancer Institute, Vol. 98, No. 5, March 1, 2006
Consider if the presentation of elevated PSA, urinary symptoms, with the addition of a “diagnostic” ultrasound confirming size and shape (morphology) was taken into consideration to confirm or rule-out BPH. A diagnosis of BPH would be confirmed. There would be no requirement of a biopsy until the BPH and its symptoms was either resolved or at minimum stabilized. With such a diagnosis LS could then be treated with a nutritional support plan with followup in 3 months. He may have had the opportunity to defer those uncomfortable biopsy procedures indefinitely.
Without continued, periodic biopsy procedures, would there be a risk of missing a life-threatening, high-risk prostate cancer? It would be reasonable to continue periodic PSA tests, investigate any change in symptoms or prostate volume. If the patient continues a maintenance nutritional program and PSA is elevated or increases without a corresponding increase of symptoms or prostate enlargement, there would be justification for increased scrutiny. The appropriate and justified next step would an MRI of prostate exam (magnetic resonance imaging).
Now that LS has been diagnosed with cancer, the best course of action begins with MRI of prostate exam. Biopsy procedures are documented to have poor accuracy, finding cancer in less than 30% of attempts. Additionally, LS has an extremely large prostate. The ultrasound imaging device cannot adequately image a prostate of this size. Due to “signal fall-off” the urologist can only visualize about half of the gland. Even if the urologist could see the entire prostate, his biopsy device on the ultrasound probe does not have the capability to reach to the anterior regions of the gland. The best results can only capture tissues cores of about 1 inch in length. According to LS’s pathology report, the average length of tissue cores was ~1cm, meaning that the needle penetrated <¼ the depth of his prostate.
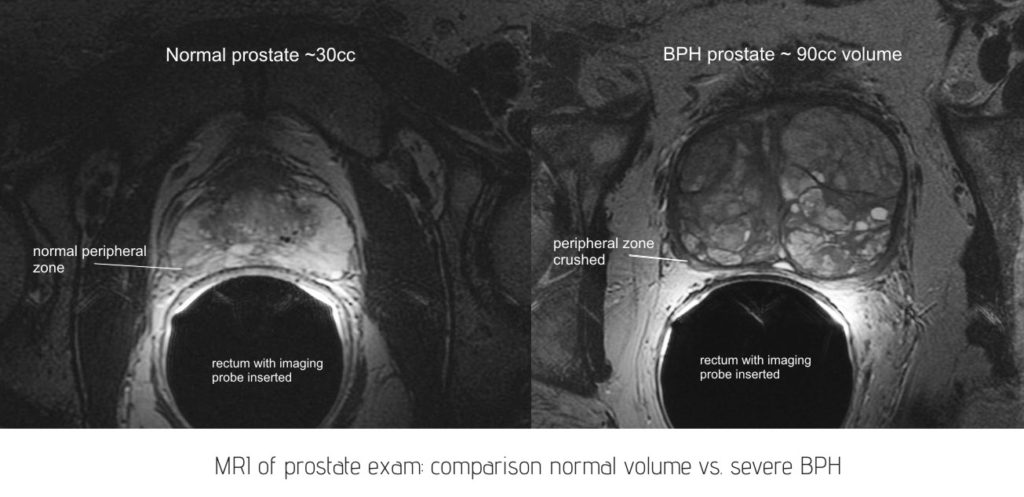
MRI of Prostate
An MRI exam would provide the ability to accurately image the entire prostate with very high quality. This harmless imaging device can also sample actual function of tissue revealing tissues at-risk for, or suspicious of cancer. With a radiologist experienced in MRI of prostate, the exam can provide a very high confidence level regarding the risk of cancer, classify these regions and inform regarding the overall health of the gland. The MRI image comparison above demonstrates modern MRI system’s excellent image quality and diagnostic value. The image on the right is representative of LS’s prostate. It becomes very apparent that this condition would produce urinary symptoms. The bladder is located just above the prostate with the urethra passing through the center of the gland.
Awareness of this specialized MRI exam of the prostate, and its utilization has increased in recent years. Even though, it is not that common. It requires special approval from insurance providers to pay for the exam. The MRI exam was approved and scheduled. The exam was performed and interpretation confirmed a region suspicious for cancer. Curiously, the region identified by the MRI unit was on the wrong side of the prostate. The left side. The biopsy analysis that identified the low-risk cancer, located the cancer on the right side of the prostate. This could mean that the MRI discovered a suspicious region that was missed by the previous 3 biopsy procedures. It happens. The MRI did not identify regions suspicious for cancer on the right side of the gland, probably due to the fact it is a tiny cancer. The MRI reveals the reason why the cancer tissue recovered was “fragmented” with small area of cancer, only “0.8 mm” length. In the example above, on the right, the peripheral zone, where the majority of cancers are diagnosed, is compressed by the hyperplasia down to about 1 mm. The urologist and pathhologist were unaware of this important anatomical detail. The radiologist recommended that the patient be scheduled for an MRI-guided, targeted biopsy. This procedure takes only 2-4 cores that are targeted only to the suspicious region(s).
From the Radiologist’s MRI report:
“One small focal suspicious lesion, however, was identified in the mid left peripheral zone …advanced diffusion restriction shown which is typically seen in more aggressive cancers (typically Gleason 7 or greater). Total PIRADS for this lesion would be 4, clinically significant cancer is likely to be present.” Radiologist’s interpretation
The patient subsequently had difficulty getting time off from work to schedule the second MRI for the targeted biopsy. Time went by until the patient was able to take time off in December. The radiologist expressed that too much time had passed and the patient would need to be re-scanned by the MRI prior to performing the targeted biopsy. The patient could be scanned the first day and have the biopsy procedure the next day. We will see that it was providence that LS was unable to get time off work with the resulting requirement to repeat the MRI exam!
The second MRI exam was performed in December. LS had been on the nutritional support regimen for 6 months. While reviewing the images from the MRI exam, the radiologist noted something very unexpected – he could not find any areas suspicious for prostate cancer. All areas identified in the prior MRI exam had been “resolved.” There was no prostate cancer, no areas indicating a risk of prostate cancer
Radiologist’s report, 2nd MRI exam:
“Complete normalization of the appearance of the peripheral zones bilateral since the prior scan. There are no abnormalities identified… No suspicious lesions identified in either peripheral zone for focal prostate cancer.”
It does happen that patients’ cancers resolve themselves, that is the body heals itself over time. Some cancers do disappear. Aside from this possibility, it may be more reasonable to assume that by taking the special supplements formula consistently for six months, LS gave his body a sufficient quantity of effective resources (nutritional agents) to resolve the cancer on its own. The nutritional regimen was also successful in treating symptoms caused by his severely enlarged prostate (BPH). LS’s serum PSA had stabilized and urinary symptoms significantly improved. He was also now sleeping through the night. The patient’s PSA levels were reduced and symptoms were significantly improved. Additionally, there is extensive support in published research that nutritional agents do, in fact reduce and eliminate cancers. It is entirely reasonable to conclude that in our case, the nutritional therapy did in fact resolve both cancer lesions. Incidentally, this was not our first experience with this phenomenon.
Improved urinary symptoms, “cancer resolved”
LS had dedicated himself to following his nutritional support regimen as directed by his PA. He had been scheduled to receive a radical prostatectomy for arguably, an insignificant cancer. By making the decision to delay surgery a few months and take nutritional support, the question became moot. According to the MRI results and interpretation, LS’s cancer was resolved. There will be no surgery. He will not have to experience major surgery with the real potential of incontinence or impotence (common side effects of the surgery). Is LS’s case a fluke? The science says otherwise. LS will continue to get a PSA test every year. He will remain diligent. Regardless of any debate, LS’s example demonstrates that “early detection” of prostate cancer should not always lead to “early treatment.”
Overtreatment and MRI
Conservatively, over 1 million prostate biopsies are performed in the U.S. each year (Johns Hopkins Medicine, 2011). About 75% of those return negative result for cancer (Journal of Clinical Oncology, 2010). A significant percentage of these negative biopsies are repeated, as in our example with LS’s case who endured a total of 3 biopsy procedures only to find a “microscopic,” very low-risk cancer. These low-risk cancers represent up to 50% of all cancers diagnosed, and unfortunately, the majority of these are treated with surgery or radiation. These treatments have been widely described as “overtreatment” of the disease. The treatments are very expensive. The side effects are for life and can be devastating to men and families (incontinence, impotence, depression, lack of libido, fear of recurrence, etc.).
“We have a Prostate Cancer crisis. The lack of accurate imaging leads to a staggering number of unnecessary biopsies and treatments.”
Bringing Prostate Cancer into the Light
Faina Shtern, MD, CEO, Admetech Foundation
SNM, Center for Molecular Imaging, Innovation and Translation
http://www.admetech.org/2011/02/
MRI of prostate should be first-line diagnostic tools when a patient is identified to be at-risk for prostate cancer. It is non-invasive, painless, harmless. For men with a persistent elevated PSA serum level relevant to their prostate volume, an MRI of prostate exam should be readily available to healthcare providers. If the MRI results in any suspicious lesions identified, an image-guided target biopsy could then be considered. As it stands at present, and or the last 20 years since the introduction of MR of prostate, once a patient is referred to urology, the first-line diagnostic tool remains ultrasound-guided, prostate needle biopsy. Once the patient crosses this threshold, his life has changed. There is no turning back. A negative biopsy simply means, due to the inaccuracy of the procedure, that a danger cancer may still exist and another biopsy is required.
In our opinion, LS should never have received a single biopsy. He should not have been diagnosed with an insignificant cancer. He should not have been scheduled for surgery. Due to the fear generated by an “incurable” disease like prostate cancer, even for cancers that are low-risk, too many men are convinced to choose “early treatment.”
